Tourette’s syndrome (TS) was first described in the 19th century by the French neurologist Georges Gilles de la Tourette. It is a neuropsychiatric disorder with a genetic component characterised by sudden, brief and intermittent movements (motor tics) or vocalisations (auditory tics). Tics appear in childhood, generally between the ages of 6 and 8, and are almost always (85% of cases) subsequently associated with one or more psychiatric disorders: attention deficit with or without hyperactivity, obsessive-compulsive disorders, rage attacks, autism spectrum disorders, learning disorders, etc.
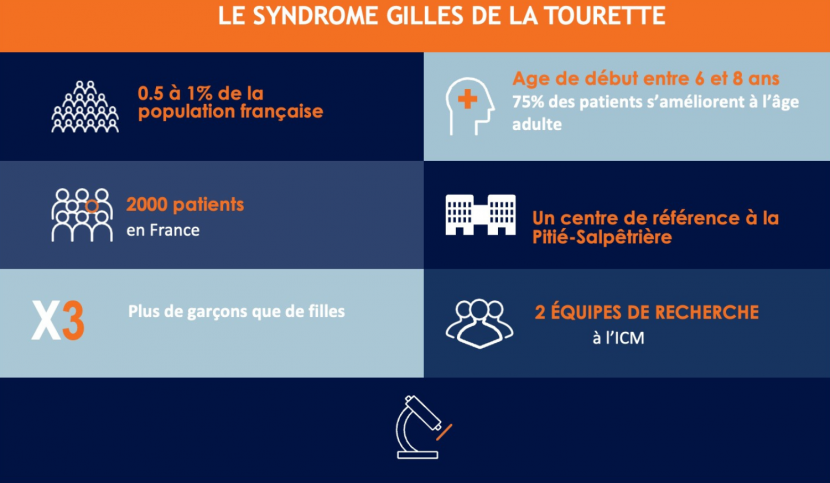
Tourette syndrome affects around one in 200 people in France (around 0.5% of the population), and more often boys than girls.
Another feature of this syndrome is that it resolves or improves spontaneously in adulthood in around 75% of patients. For the remaining 25%, symptoms may persist or even worsen. One of the challenges in this disease is therefore to understand why some patients improve spontaneously, so that we can develop therapeutic strategies to help the others.
The causes and biological mechanisms of Tourette syndrome
The precise mechanisms behind the symptoms of Tourette syndrome are still poorly understood, but the region of the basal ganglia / basal ganglia, deep structures in our brain, is particularly involved in the generation of tics. Research at the Brain Institute aims to pinpoint the brain regions responsible for the symptoms in order to tailor therapies.
There is a genetic component to GTS, but to date few predisposition genes have been identified. In fact, the risk of developing the disease for a patient’s relatives is higher than for the general population. There are probably also environmental risk factors, which have not yet been identified: we are therefore talking about a multifactorial syndrome. Teams at the Institut du Cerveau are members of international genetics consortia conducting large-scale research to identify the genetic variants associated with this syndrome.
Symptoms of Tourette syndrome
Tourette syndrome is characterised by a combination of motor and vocal tics lasting for more than a year in an individual under the age of 18, according to DSM-5 criteria. Tics vary greatly from one individual to another. Motor tics generally appear first and mainly affect the upper body, face, head and arms. They may then be followed by vocal tics. Coprolalia, often caricatured as the repetition of insults, occurs in less than 20% of patients with Tourette syndrome.
The psychiatric symptoms associated with Tourette syndrome are mainly attention deficit with or without hyperactivity, obsessive-compulsive disorder and autism spectrum disorder.
Diagnosis of Tourette syndrome
The diagnosis of Tourette syndrome is based on the evaluation of patients’ symptoms by clinical examination alone. Additional examinations such as magnetic resonance imaging (MRI) or electroencephalograms are rarely necessary, and their purpose is to rule out other pathologies. A tic frequency and intensity rating scale (YGTSS) is used to measure the severity of the disease. The search for diagnostic and prognostic markers for this disease is a key challenge for researchers and clinicians at the Institut du Cerveau.
Treatments for Tourette syndrome
Tourette syndrome can be treated in a number of ways, depending on the patient’s clinical profile and the severity of the tics. Behavioural psychotherapies aimed at treating tics are the first-line treatment according to European and American recommendations. They are aimed at all patients, regardless of the severity of their tics, but require regular exercise over a period of several months. At present, such therapy is often not feasible due to a lack of trained professionals. In these cases, we turn to drug treatments, primarily neuroleptics, to improve patients’ day-to-day lives and their integration into school or the workplace. Regular psychotherapy, speech therapy and psychomotor therapy are also recommended, depending on the associated disorders. Finally, deep brain stimulation can be offered in the most severe cases that are resistant to behavioural therapies and medication.
Last updated May 2024.