The psychological mechanisms of OCD
The psychological mechanisms of OCD are fairly well known and identified. The majority of obsessive-compulsive behaviours are linked to irrational fears about danger or risk to themselves or those around them. Patients always feel a sense of responsibility or even guilt about what might happen to them, and are overly invested in their own safety and that of others.
These fears lead to obsessions, recurring thoughts or images that are unwanted and highly anxiety-provoking, most of which relate to the dramatic consequences that possible errors in the patient’s behaviour or actions could have in terms of accidents or death.
Most OCD patients are aware that their obsessions are unrealistic but are unable to escape them.
The compulsive ritual mechanisms of OCD
To reduce or even eliminate these obsessions, patients set up compulsive ritual mechanisms, which have to be carried out in a precise manner. The irrational fear of contamination by viruses or bacteria, for example, can lead OCD sufferers to engage in excessive repetitive behaviour, such as washing their hands for at least 2 hours a day or showering according to a very precise protocol, soaping each armpit 17 times and each foot 20 times, starting with the right, and repeating the ritual from the beginning if they make the slightest mistake or lose count.
These rituals can lead the patient to devote more than 8 hours a day to them, resulting in social isolation, loss of employment and suffering for those around them.
Working, eating and meeting other people become very difficult activities. If we take the example of driving a car, some patients have to retrace their steps 20 times to make sure they haven’t killed anyone along the way, and they also have to check several media outlets over a period of several days to make sure there have been no accidents during their journey.
Here again, as with obsessions, most patients with obsessive-compulsive disorder (OCD) are aware that they are not going to die of an infection if they don’t soap each armpit 17 times, but the need to perform these rites is irrepressible in order to calm their anxiety and fear.
These obsessive-compulsive behaviours trap patients in a vicious circle: the obsession leads to a ritual, which once performed generates new obsessions.
From a more scientific point of view, this behavioural dysfunction seems to stem from what researchers call “pervasive doubts”, which are probably due to a disturbance in the control of uncertainty involved in decision-making.
Research into the causes of OCD at the Paris Brain Institute
The “Neurophysiology of repetitive behaviours” team, led by Eric BURGUIERE, a CNRS researcher, is seeking to identify the brain dysfunctions at the root of this pathological doubt and to understand why and how repeated behaviours appear and become “automated”.
Thanks to a translational approach in experimental models and in OCD patients, and using brain imaging, the researchers in this team have highlighted the essential role of two brain regions in this pathology.
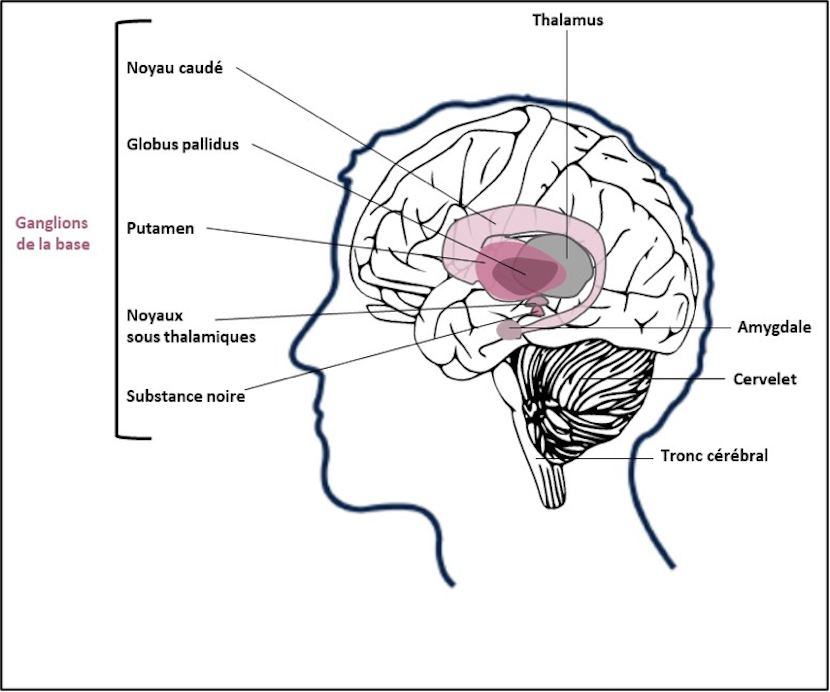
The orbitofrontal region is involved in the appearance of the pervasive doubt at the origin of the repetitive checking behaviours, while deeper regions of the brain known as the ‘basal ganglia’ are more involved in the management of emotions.
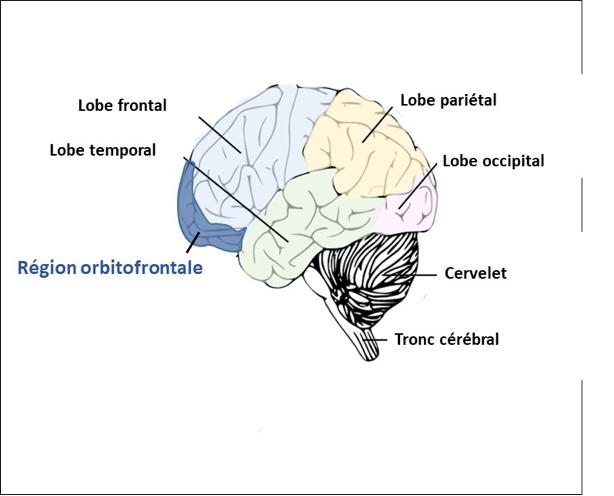
The aim of this research team is also to understand how the activity of neurons in these regions is disrupted in obsessive-compulsive disorder.
Using functional magnetic resonance imaging (fMRI) and magnetoencephalography (MEG) recordings, the researchers showed that neuronal activity in these areas of the brain was greatly increased in patients with OCD.
fMRI is a brain imaging technique that measures the activity of neurons in brain areas that are stimulated when the person performs a task such as reading, moving a limb or looking at images, by measuring the increase in blood flow in these areas.
MEG can also be used to measure brain activity during the performance of a task by measuring the electromagnetic field emitted by active neurons.
One hypothesis to explain this hyperactivation of these brain regions is based on a disturbance in the levels of neurotransmitters (molecules essential for the passage of information from one neuron to another) such as serotonin, dopamine and vasopressin.