Although COVID-19 is considered to be primarily a respiratory disease, SARS-CoV-2 affects multiple organ systems including the central nervous system (CNS). Yet, there is no consensus on the consequences of CNS infections. Here, we used three independent approaches to probe the capacity of SARS-CoV-2 to infect the brain.
First, using human brain organoids, we observed clear evidence of infection with accompanying metabolic changes in infected and neighboring neurons. However, no evidence for type I interferon responses was detected. We demonstrate that neuronal infection can be prevented by blocking ACE2 with antibodies or by administering cerebrospinal fluid from a COVID-19 patient. Second, using mice overexpressing human ACE2, we demonstrate SARS-CoV-2 neuroinvasion in vivo.
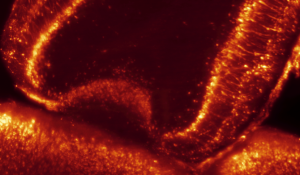
3d by sheet imaging that shows the presence of the virus in the neurons of the olfactory bulb
Finally, in autopsies from patients who died of COVID-19, we detect SARS-CoV-2 in cortical neurons and note pathological features associated with infection with minimal immune cell infiltrates. These results provide evidence for the neuroinvasive capacity of SARS-CoV-2 and an unexpected consequence of direct infection of neurons by SARS-CoV-2.
Reference:
Neuroinvasion of SARS-CoV-2 in human and mouse brain, Eric Song, Ce Zhang, Benjamin Israelow, Alice Lu-Culligan, Alba Vieites Prado, Sophie Skriabine, Peiwen Lu, Orr-El Weizman, Feimei Liu, Yile Dai, Klara Szigeti-Buck, Yuki Yasumoto, Guilin Wang, Christopher Castaldi, Jaime Heltke, Evelyn Ng, John Wheeler, Mia Madel Alfajaro, Etienne Levavasseur, Benjamin Fontes, Neal G. Ravindra, David Van Dijk, Shrikant Mane, Murat Gunel, Aaron Ring, Syed A. Jaffar Kazmi, Kai Zhang, Craig B Wilen, Tamas L. Horvath, Isabelle Plu, Stephane Haik, Jean-Leon Thomas, Angeliki Louvi, Shelli F. Farhadian, Anita Huttner, Danielle Seilhean, Nicolas Renier, Kaya Bilguvar, Akiko Iwasaki, Journal of Experimental Medicine, January 2021.
J Exp Med (2021) 218 (3): e20202135.







