Over the past fifteen years, neurosurgeons have been perfecting a fascinating technique: using ultrasound to temporarily open the blood-brain barrier to facilitate the action of therapeutic molecules in the central nervous system. At Paris Brain Institute, Séverine Boillée’s team, in collaboration with Professor Alexandre Carpentier from the neurosurgery department at the Pitié-Salpêtrière hospital and the startup CarThera, have demonstrated that this technique can also be applied to the blood–spinal cord barrier. And in motor neuron disease, ultrasound treatment alone could be a promising avenue! These pioneering results, obtained in mice, are published in eBioMedicine.
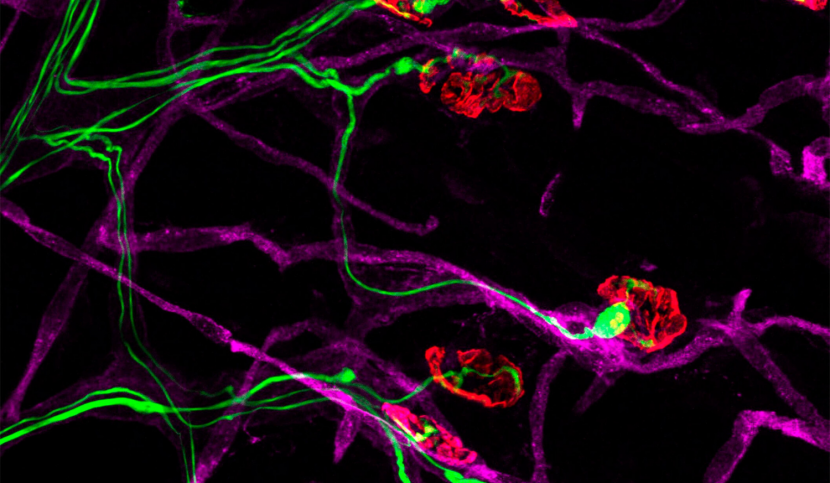
Most drugs cannot cross the blood-brain barrier, the natural border that protects the central nervous system from potentially toxic substances circulating in the bloodstream. But they are also held in check by a lesser-known adversary: the blood-spinal cord barrier—made up of small blood vessels—which plays a similar role around the spinal cord.
“These natural barriers are a major obstacle to the development and evaluation of new drugs in neurology,” explains Séverine Boillée (Inserm), a researcher at Paris Brain Institute. “In amyotrophic lateral sclerosis (ALS), or motor neuron disease, we constantly seek new techniques to help therapeutic molecules reach the motor neurons.”
Indeed, amyotrophic lateral sclerosis causes the progressive degeneration of motor neurons, the cells that control the body’s voluntary muscles. Located in the cerebral cortex and the anterior part of the spinal cord, their destruction causes progressive paralysis of the limbs and the muscles that control breathing and swallowing.
Opening a pathway to motor neurons
Previous research* has shown that it is possible to temporarily open the blood-brain barrier by injecting microbubbles into the bloodstream: these vibrate under the effect of low-intensity ultrasound, inducing mechanical stress on the vessel walls. The blood-brain barrier is then disrupted, allowing therapeutic molecules to pass into the brain for a few hours.
Séverine Boillée and her colleagues, in collaboration with Prof. Alexandre Carpentier (AP-HP, Sorbonne University), are the first to precisely evaluate the efficacy and safety of this technique in motor neuron disease, this time targeting the spinal cord. Their aim? Administering to ALS mice a treatment that has already demonstrated its potential in animals—the growth hormone IGF1—as close as possible to the motor neurons.
To facilitate the therapeutic molecule’s action, the researchers used pulsed ultrasound once a week for five weeks in the animals’ lumbar region. Their results are encouraging: a single session resulted in a high concentration of IGF1 in the spinal cord. After five weeks, the animals treated with ultrasound had a longer life expectancy than those who had received growth hormone alone, or a placebo.

A 1 MHz ultrasound transducer was positioned to target the mouse’s lumbar spinal cord. Pulsed ultrasounds were administered for 150 seconds at the same time as the microbubbles. Credit: Paris Brain Institute (CC BY 4.0).
An unexpected phenomenon
“We also observed a surprising phenomenon. The mice that received ultrasound without medication lived longer than the controls,” explains Séverine Boillée. “In other words, ultrasound alone was effective in slowing the progression of the disease, whereas IGF1 showed no benefit.”
What if pulsed ultrasound could be used as a therapeutic tool in amyotrophic lateral sclerosis? Of course, further studies will be needed to understand the mechanism that enabled the mice to live longer. But the team is already on to something: ultrasound may have affected immune cells.
“The tools we need to use ultrasound in the human spinal cord must now be developed,” adds the researcher. However, the clinical tools that allow us to intervene in the brain are already there: Prof. Alexandre Carpentier, Prof. Gaëlle Bruneteau (AP-HP), a neurologist at the ALS Centre in Paris, and the start-up CarThera will shortly be launching the SonoSLA therapeutic trial; it will assess the absence of ultrasound toxicity and the tolerance of the device in ALS patients, followed by its efficacy on symptoms. “This strategy could open up real therapeutic prospects for patients,” concludes Séverine Boillée.
Funding
This study was funded by the Laboratoire de Recherche en Technologies Chirurgicales Avancées (LRTCA), the Foundation for Medical Research (FRM), the French Society of Neurosurgery (SFNC), the Fonds d’Études et de Recherche du Corps Médical (FERCM) of the Paris hospitals, l’Aide à la Recherche des Maladies du Cerveau (ARMC), SLA Fondation Recherche (SLAFR), and the Investments for the Future program.
Declaration of interests
Alexandre Carpentier is a consultant for the university start-up CarThera, which he founded. He has interests in the company and has filed patents held by Sorbonne University relating to the results presented in the article.
Reference
Montero, A. S. et al. Effects of ultrasound-mediated blood-spinal cord barrier opening on survival and motor function in females in an amyotrophic lateral sclerosis mouse model. eBioMedicine, Juillet 2024. DOI: 10.1016/j.ebiom.2024.105235
Bibliography (*)
Carpentier, A. et al. Repeated blood-brain barrier opening with a nine-emitter implantable ultrasound device in combination with carboplatin in recurrent glioblastoma: a phase I/II clinical trial. Nature Communications, Février 2024. DOI: 10.1038/s41467-024-45818-7
Sonabend, A. M. et al. Repeated blood-brain barrier opening with an implantable ultrasound device for delivery of albumin-bound paclitaxel in patients with recurrent glioblastoma: a phase 1 trial. The Lancet Oncology, Mai 2023. DOI: 10.1016/S1470-2045(23)00112-2
Carpentier, A. et al. Clinical trial of blood-brain barrier disruption by pulsed ultrasound. Science Translational Medicine, Juin 2016. DOI: 10.1126/scitranslmed.aaf60